Euthanasia and saying goodbye to a beloved pet and family member is a very difficult decision to make, no matter who you are. As a veterinarian, it is something that we have to deal with as a part of our daily routine.
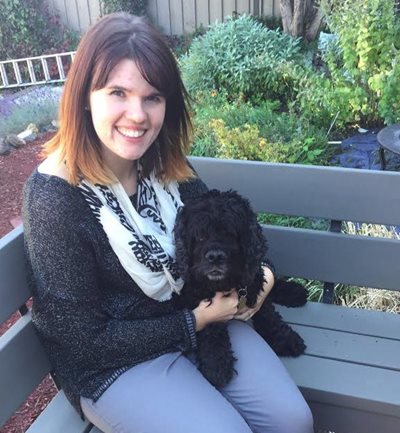
This could be in the form of counselling a client who is having a hard time deciding “is it time,” giving a terminal diagnosis and discussing palliative management or conducting the euthanasia procedure itself. It is a terrible part of our job; however, I feel fortunate that I can end the suffering of a beloved pet and prevent their family from watching them live in pain. As much as this is routine for us, it did not help prepare me – nor does it ever – for having to decide for my dog, my Mac.
On December 7th, 2017, I brought Mac into the clinic to surgically remove some warts that were bothering him. As part of his pre-screening for surgery, I elected to perform a full comprehensive blood panel – I almost didn’t, but boy am I glad I did! I was shocked to see that Mac’s blood levels were extremely abnormal – he had no platelets (essential for helping blood clot) and his red blood cell number was very low and creeping into a worrisome anemia. These are not good things for any dog, especially for one about to go “under the knife.” Wart surgery was aborted and instead, we started to do some more diagnostics to try to figure out why his platelet and red blood cell numbers were so low.
The veterinarian in me could list our top differentials: immune-mediated condition (where his body is destroying his healthy cells), a tumour or cancerous process or a possible trauma/internal wound that was consuming or using up all of his platelets. Given Mac’s ripe old age of 12.5 years, the most likely diagnosis was either an immune-mediated disease or a destructive process. Our diagnostics did not yield an obvious tumour but it was still a possible concern. We elected to treat him like he had an immune-mediated condition and started him on an immunosuppressive dose of steroids. Mac became a frequent flyer at the clinic on both working days and my days off because, with a condition like his, it is critical to constantly be looking at his blood to see if there is an improvement, or if the values are dropping. Initially, Mac responded well to the steroids, but about one week in, we had to add in another immunosuppressive agent. Fortunately, within a few days, Mac’s blood levels were up and he was more energetic and acting like himself again. These medications allowed us to spend one last Christmas with Mac and our families. I was so fortunate throughout this time to work with the fantastic people here at Kamloops Veterinary Clinic. They helped to both comfort and counselled me on the best course of action and next steps for Mac.
Yes, this is what I do, but sometimes when it is your own pet, you need to take a step back and have help seeing the bigger picture. Given Mac’s age and likely reason for his condition we knew our time with him was becoming limited, but as a family, we decided to keep him on the medications for as long as he was comfortable, happy and had a good quality of life.
Making quality of life discussions are a very common part of the conversation I have with clients about the end of life decisions for their four-legged family members. The Collins English dictionary defines the quality of life (QOL) as “the general well-being of a person… defined by health and happiness” and this definition is used in the same context for our pets.
QOL includes the ability of our pets to eat and drink, go the bathroom freely without issues, be able to move around freely and to be able to enjoy every day. For our pets, QOL also includes their interactions with the family – are they still with everyone or are they secluding themselves in a separate room? Do they even get excited to greet family when they get home or new people at the door Do they still do the same things they have done since they were younger? These are just some of the necessary measures of quality of life that we can all use for our pets, and these steps are as individual as the pet themselves.
When making these difficult decisions, I recommend sitting down as a family and making a list of what makes a great day for your pet; is it getting to chase a ball (no matter how slow they may be in the end)? Or, is it being able to comfortably cuddle-up on their favourite lap? Is it getting to greet each person who comes through the door? And when we have this list, how many of these things can we check off each day? Is our pet able to achieve most of these, or are the items on their list that make a great day becoming fewer and fewer? I think these lists help us to be somewhat objective in a very emotional decision. These lists allow us to ensure that we are achieving the best quality of life we can for our pets – our family.
In some cases, you just know, or they tell you in their way they are ready to let go. Mac let me know on the night of January 8th that it was his time. I took him to the clinic where I have the most wonderful co-workers who let me say goodbye to his family and not his vet. He passed peacefully in my arms, cuddled up like any other night, without any pain and surrounded by love.
I wish we could keep them with us forever, but unfortunately, that is not possible. We must remember the good times we had, and though their time is short, know that we were so lucky to have had them and their unconditional love in our lives. It may be one of the hardest decisions we have to make, but it is by far our most compassionate one – to let them go peacefully, without any suffering.
This is not an easy decision to make, but when it comes time, please know we are here to help.
Goodbye, Mac.

Written by Dr. Tara MacKay D.V.M.